The Opioid Vaccine: How Nanoparticles Can End Overdose Deaths
Opioid Vaccine, a nanoparticle-powered immunization could train the immune system to block opioids like fentanyl from reaching the brain—potentially preventing overdoses and reshaping addiction treatment.
The opioid crisis steals lives daily—but what if a vaccine could stop overdoses before they happen? Scientists are using nanoparticles to train the immune system to block deadly opioids like fentanyl, offering a revolutionary shield against tragedy. This isn’t science fiction—it’s the cutting edge of addiction medicine. Dive into the science, the hope, and the hard ethical questions behind the opioid vaccine.
Table of Contents
🌎 The Opioid Crisis in Numbers
100,000+ Deaths/Year
Drug overdoses in the U.S., driven largely by synthetic opioids like fentanyl.
4× in 20 Years
There has been a fourfold increase in overdose deaths over the last two decades.
18–45 Years Old
Fentanyl is a leading cause of death among Americans aged 18–45.
Sources: CDC, NIH, peer-reviewed studies—full citations below.
🧬 A New Hope: The Opioid Vaccine
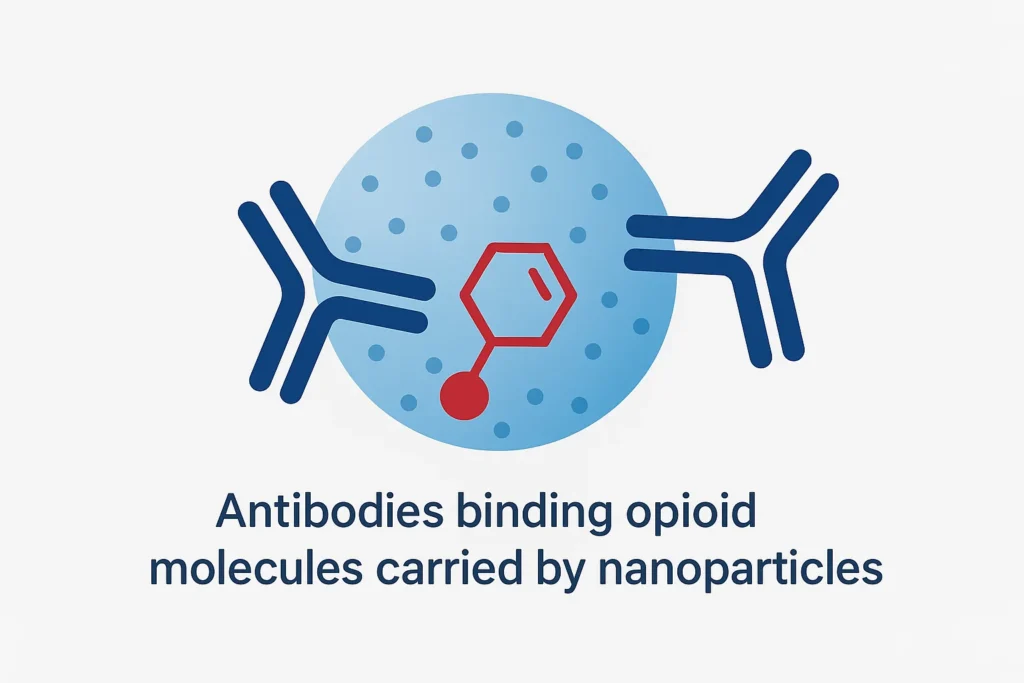
The concept: train your immune system to recognize opioid molecules. When exposure happens later, antibodies bind the drug in the bloodstream so it can’t cross the blood-brain barrier to cause euphoria—or lethal respiratory depression. Designing the precise structure of the vaccine’s components—ensuring the opioid hapten is presented correctly to the immune system—relies on advanced understanding of protein interactions, a field recently revolutionized by AI-powered structural biology.
How it works
- Nanoparticle delivery: Researchers attach an opioid-like hapten to a nanoparticle or carrier.
- Immune training: Your immune system produces specific antibodies.
- Neutralization: If opioids are taken later, antibodies bind them in the blood.
- Brain protection: Bound drug can’t cross the blood-brain barrier—no high, no overdose.
Different from methadone or buprenorphine, which manage cravings; the vaccine blocks the drug’s effect.
“If this vaccine had been around three years ago, I might have gotten clean sooner… or maybe I wouldn’t have been ready. Recovery isn’t just about blocking a high—it’s about rebuilding a life.”
— Rachel, in recovery
The Science Behind the vaccine: More than just Nanoparticles
While the summary of how the Opioid vaccine works is clear, the real magic—and the key challenge for scientists—lies in the molecular details. It’s not just about using nanoparticles; it’s about how they are engineered to train the immune system with unprecedented precision.
The core strategy is called hapten-carrier conjugation. Opioid molecules on their own are too small to be recognized by the immune system. To solve this, researchers chemically attach a stable, opioid-like molecule (called a hapten) to a larger, harmless carrier protein that the immune system already knows how to attack—like a piece of the tetanus toxin. This combination tricks the body into seeing the opioid hapten as a serious threat.
This is where the nanoparticles come in, and their role is more sophisticated than just being a simple carrier. As detailed in a pivotal 2024 study published in Angewandte Chemie, the nanoparticle functions as a precision delivery system for critical immune-boosting compounds called adjuvants.
Think of it like this:
If the hapten-carrier complex is the “mugshot” of the enemy, the nanoparticle is the delivery truck that brings an alarm bell directly to the immune system’s headquarters. The adjuvant is the alarm bell itself. Without this powerful alarm, the immune system might glance at the mugshot and forget it. But with the nanoparticle ensuring the adjuvant is delivered right to the right cells, the immune system goes on high alert, creating a legion of highly specific and persistent antibodies against the opioid.
This elegant engineering—using tunable polymer nanoparticles to control the delivery of adjuvants—is what allows the vaccine to produce the strong and long-lasting immunity needed to be effective. It’s a leap beyond simple concepts to a modular, programmable platform for vaccine design.
🔬 What the Research Shows
Highlights: Early-stage studies report strong antibody responses, drug neutralization in blood, and prevention of fentanyl’s effects in animals. NIH’s HEAL Initiative funds multiple vaccine programs. Some candidates are preparing for or entering first-in-human testing.
Development timeline
Preclinical
Design & animal models
Phase I
Safety in healthy volunteers
Phase II
Dosing & immunogenicity
Phase III
Efficacy at larger scale
FDA Review
Approval pathway
Why it could be a game-changer
- Overdose protection even if relapse occurs.
- Long-lasting antibody response (months in preclinical models).
- Works alongside existing treatments and harm-reduction tools.
- Potential protection for high-risk groups and first responders.
⚖️ The Ethical Debate
Consent & autonomy
Should vaccination be purely voluntary, especially for justice-involved individuals? Transparent consent is essential.
Reversibility & medical care
Antibodies can persist. Care plans for surgery and acute pain must be arranged if opioids are blocked.
Specificity to each opioid
Fentanyl, heroin, and oxycodone may require distinct vaccines, complicating rollouts.
Public trust
Vaccinating to address a behavioral health issue is novel; clear community engagement matters.
Limitations and the Path Forward
While the promise of an opioid vaccine is immense, it is crucial to view it not as a magic bullet, but as a potential breakthrough within a broader medical toolkit. Understanding its limitations is key to defining its realistic role in combating the opioid crisis.
Key Limitations
First, it is vital to recognize what the vaccine does not do. It does not address the underlying psychological addiction or cravings. The vaccine is a form of pharmacokinetic intervention—it blocks the drug’s effect in the body. It does not, however, repair the neurological pathways of addiction or the behavioral patterns that drive substance use. A vaccinated individual would still experience intense cravings and would need robust psychological support to achieve recovery.
Second, these vaccines are highly specific. A vaccine designed against fentanyl will not protect against an overdose from oxycodone, heroin, or other substances. This is a significant limitation in an era of polysubstance use, where individuals often encounter drugs mixed with unexpected synthetic opioids. This specificity means the vaccine is a shield against a specific threat, not an impenetrable barrier.
The Path Forward: Combination Therapy
Given these limitations, the future of an opioid vaccine lies squarely in Combination Therapy. Its greatest potential will be realized when used alongside existing, evidence-based treatments.
Imagine a treatment plan where:
- The opioid vaccine provides a physiological safety net, preventing overdose and reducing the rewarding effects of a specific opioid.
- Medications like Methadone or Buprenorphine (MOUD) manage withdrawal symptoms and curb cravings at the neurological level.
- Behavioral counseling addresses the psychological and social factors of addiction
This multi-pronged approach attacks the problem from every angle. This principle of managing a powerful treatment’s limitations is a common theme in modern medicine. For instance, the remarkable success of GLP-1 drugs like Ozempic for weight loss comes with the challenge of mitigating unintended side effects, such as muscle loss, requiring a combined strategy of diet and exercise.
In this context, the opioid vaccine would not replace current treatments but would augment them, offering an additional layer of protection that could be lifesaving during a lapse or relapse. Its development signals a move toward more integrated and personalized strategies for treating substance use disorder.
📌 The Ultimate Takeaway
The opioid vaccine will not be a standalone cure for addiction. Its promise, however, is profound. By acting as a biological shield against overdose, it could become a cornerstone of a modern, compassionate, and multi-layered defense strategy. When integrated with prevention education, robust treatment options like medication-assisted therapy, and harm-reduction tools, this scientific breakthrough has the potential to turn the tide, saving thousands of lives and creating crucial windows of opportunity for recovery.
🔗 References
- GAO. Science & Tech Spotlight: Opioid Vaccines. gao.gov
- Nature npj Vaccines (2023). Anti-fentanyl vaccine with TLR7/8 adjuvant. nature.com
- UC Davis CNPRC. Oxycodone VLP vaccine. cnprc.ucdavis.edu
- Sci. Direct (2022). Anti-oxycodone vaccine safety. sciencedirect.com
- NIH HEAL Initiative. Opioid vaccine projects. heal.nih.gov
- Boston Children’s. Fentanyl vaccine acceptability. answers.childrenshospital.org
- Verywell Health. University of Houston fentanyl vaccine. verywellhealth.com
- U. Maryland Fischell Institute (Seminar). LNP-templated anti-opioid vaccine. fischellinstitute.umd.edu
- Wiley Angew. Chem. (2024). Non-covalent LNP fentanyl hapten vaccine. onlinelibrary.wiley.com


One Comment